Risk Watch (April '18)
Selected research, publications, and resources to promote evidence-informed risk management in Canadian healthcare organizations. Prepared by HIROC. Some titles are open access while others may require a subscription or library access; the librarian at your organization may be able to assist you. Please contact riskmanagement@hiroc.com for assistance if required.
Alternate Level of Care

Bender D, Holyoke P. Healthc Manage Forum. 2018 (online, February):1-5.
Study reviewing 393 alternate level of care (ALC) patient cases across six Canadian hospitals from the home and community lens to determine the underlying causes for ALC issues. Four observations emerged: insufficient home and community supports before hospitalization; underestimation of patients’ potential for independence; general deconditioning of patients while in hospital; hospitals’ lack of understanding of home care. Recommendations for reducing the incidence of patients requiring ALC included: reinforcing the need to proactively identify and provide supports to enable patients to remain in their homes; reorienting hospital staff to help patients maintain and restore function while in hospital; collaboration between hospital and community providers on integrated admission criteria for post-acute programs that help transition patients to homes; increasing hospital staff knowledge and experience of home and community care.
Quality Improvement / Documentation
‘Take Ten’ improving the surgical post-take ward round: a quality improvement project

Banfield D, Adamson C, Tomsett A, et al. BMJ Open Qual. 2018 (online, March):1-5.
Quality improvement project by junior doctors in a post-surgical unit of a UK hospital to improve the documentation of patient management plans. Process mapping identified ten important points in the assessment and management of a surgical patient: observations; examination; impression of diagnosis; investigations; antibiotics; IV fluids; VTE risk assessment; nutrition status; estimated length of stay; ceiling of treatment. A checklist with the ten points to guide team discussions and documentation was introduced. After three PDSA cycles, results showed documentation improved the most in impression and investigations (from 60% to 87.5%). Three years after the introduction of the checklist, overall compliance remained high and after engagement of the wider multidisciplinary team, it was found that nursing staff were, in fact, the key drivers to sustaining checklist use.
Quality Improvement / Large Scale

Britto M, Fuller S, Kaplan H, et al. BMJ Qual Saf. 2018 (online, February):1-10.
Article describing improvement in outcomes through a collaborative network model to achieve the vision of a Learning Healthcare System. The model was designed, developed and implemented over 13 years, with researchers, clinicians, and families, with support from US paediatric medical centers. The network framework aligned participants around a common goal of improving health outcomes, transparency of outcome measures and a flexible adaptive collaborative learning system. Authors described how the framework has been replicated, resulting in substantial improvement in outcomes with sample results from four most mature learning networks.
Safety / Speaking Up

Martin G, Aveling E, Campbell A, et al. BMJ Qual Saf. 2018 (online, February):1-8.
Study to examine the role of formal channels in encouraging or inhibiting an employee to voice quality or safety concerns. Interviews were conducted with 165 participants from a range of occupational and professional backgrounds, including senior leaders and front line staff at three academic hospitals located in two countries. Results showed that leaders reported valuing the employee voice and used formal channels such as incident reporting systems, monitoring of indicators and risk management techniques for gathering information towards resolution. However, the way the formal systems operate, authors noted some concerns were never voiced. Authors identified considerations for leaders responsible for quality and safety to complement formal mechanisms with alternative informal opportunities for listening to concerns. Article includes quotes from participants.
Ward Rounds / Patient Participation
Patient participation in inpatient ward rounds on acute inpatient medical wards: a descriptive study

Redley B, McTier L, Botti M, et al. BMJ Qual Saf. 2018 (online, February):1-9.
Study to describe patient participation during ward rounds at two tertiary hospitals in Australia. The Control Preference Scale, which is a measure for the degree of control an individual wants to assume when decisions are being made about medical treatment, was used. Patient responses were stratified into three groups of participation preferences: active control where the patient makes decisions; shared control where the patient prefers to make decisions jointly with clinicians and passive control where the patient prefers clinicians to make decisions about their care. Of the 52 patients observed over 133 ward rounds, 30.8% reported an active control preference, 25% expressed shared control preference and 44% expressed low control preference. Results showed few rounds (18%) involved patient participation in decisions about care. Analysis revealed two themes, supporting patient capability and clinician-led opportunity, contributed to patient participation or non-participation in ward rounds irrespective of control preference.
Resuscitation / Simulation

Calder L, Bhandari A, Mastoras G, et al. Int J Qual Health Care. 2018 (February);30(1):16-22.
Study to determine resuscitation team members’ perceptions of the effectiveness of the Situational Awareness Display tool (a visual cognitive aid to help detect what is going on around you) at a Canadian trauma centre. Focus groups were conducted with physicians, nurses, and respiratory therapists. Out of 33 participants, results showed the majority of participants strongly endorsed the Situational Awareness Display’s value in simulation. Themes emerged related to improved perception of patient data, comprehension of context and ability to project to future decisions regarding potential patient deterioration. Positive impacts were seen related to patient safety, provider performance and team communication. Article includes a depiction of the visual display used in simulation and representative quotes from focus group participants.
Second Victim
When clinicians drop out and start over after adverse events

Rodriquez J, Scott S. Jt Comm J Qual Patient Saf. 2018 (March);44(3):137-145.
Study to explore the experiences of healthcare providers who changed career paths as a result of their involvement in an adverse event across the US and Canada. A web-based survey was used; 77 individuals transitioned careers. Results showed 65% of healthcare providers had inadequate social support after the adverse event. Once providers changed roles, 34% felt less joy and meaning in their new roles while 20% thrived with a renewed focus on implementing patient safety initiatives including enhanced peer-support networks. Authors noted healthcare providers’ emotional reactions were consistent with organizational expectations after an adverse event happened, resulting in suppressed feelings of guilt and shame.
“Clinicians reported that the expectation among employers and coworkers, either explicitly stated or implicitly suggested, that they should regulate their emotions to suppress how they felt had a lasting impact on their careers” (p.143).
Elder Abuse
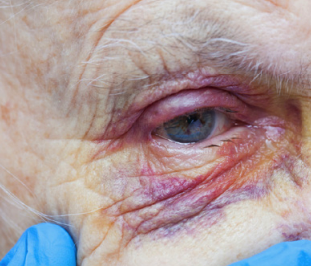
Rosen T, Mehta-Naik N, Elman A, et al. Jt Comm J Qual Patient Saf. 2018 (March);44(3):164-171.
Article describing the introduction of a multidisciplinary emergency department-based Vulnerable Elder Protection Team (VEPT) at a US academic medical centre. The VEPT was implemented to improve the identification and treatment of potential victims of elder abuse 24 hours a day/7 days a week. All emergency department providers were trained in recognizing the signs of elder abuse and the VEPT can be activated by any provider via a single page/telephone call. Initial assessment is completed by a social worker who then involves the on-call VEPT medical provider as necessary. The VEPT was launched in 2017 and has not been formally evaluated to date; evaluation is underway including examining the number of referrals and completed consultations. Outcomes will explore medical, functional, psychosocial, and legal impacts. Article includes figures depicting an overview of the team and the protocol for consultation and intervention.
Quality Improvement

Hayes C, Goldmann D. Jt Comm J Qual Patient Saf. 2018 (March);44(3):155-163.
Study to develop a model to design more adoptable quality improvement (QI) interventions. Research in two areas, diffusion of innovation and work stress, was reviewed to identify factors that influence adoptability of QI interventions, specifically as they pertain to workload and perceived value by healthcare providers. Feedback from a panel of 11 leading experts was used to refine the list of factors and the model itself. Six key elements associated with QI adoption were identified in two categories: intervention design (workload; complexity; efficacy) and implementation strategy (end-user participation; alignment and planning; resource availability). Pilot testing by 16 individuals with advanced QI knowledge found good face validity and usability for the model and supporting tools. The model has been included in several QI training program curricula in Canada and internationally. An assessment guide for the six elements is included.
Other Resources of Interest
2018 annual cybersecurity report (February 2018). Cisco (US) report presenting the latest data about attacker behaviour and recommendations for defenders (free with registration).
2018 top 10 patient safety concerns for healthcare organizations (March 2018). ECRI (US) report identifying emerging patient safety challenges, including diagnostic errors, health IT, and leadership (free with registration).
Amendments to the Long Term Care Homes Act proclaimed into force (February 2018). Borden Ladner Gervais LLP (CDN) article on Long-Term Care Homes Act amendments in Ontario proclaimed into force February 1, 2018.
Doctors learn how to talk to patients about dying (February 2018). Kaiser Health News (US) article describing the large scale effort to train physicians to have conversations with seriously ill patients.
Managing trauma patients in the community (March 2018). University of Toronto Trauma Program (CDN) 8-minute video for healthcare providers in community hospitals; includes links to transport checklists.
Minnesota hospitals report increase in preventable errors (February 2018). Star Tribune (US) article on how never events such as surgeries on the wrong body part still occur despite prevention efforts.
Opioid wisely (March 2018). Choosing Wisely Canada campaign with over 30 organizations to encourage thoughtful conversation between patients and clinicians to reduce harms associated with opioid prescribing.
Overcoming challenges in codifying and replicating complex health care interventions (February 2018). Health Affairs (US) article on the diffusion of innovation highlighting research and programs in the UK.
Patient and family engagement in Alberta Health Services: improving care delivery and research outcomes (February 2018). SAGE Public Health (US) podcast interview with patient and family engagement advisory members at Alberta Health Services.
Recent media spotlight puts long-term care on centre stage (February 2018). Borden Ladner Gervais LLP (CDN) article on the attention that follows the high profile Long-Term Care Homes Public Inquiry in Ontario.
Tracking privacy breaches in 2018 – tools and tips (January 2018). Kate Dewhirst Health Law LLP (CDN) article on new requirement to track and report privacy breaches to the Information and Privacy Commissioner of Ontario.