How MGH’s Oncology & Hematology Clinic Exemplifies the HIROC Change Maker Mentality

HIROC is always looking for stories that showcase the incredible work happening across our healthcare system – stories that remind us of what’s possible when teams put safety and continuous learning at the centre of care.
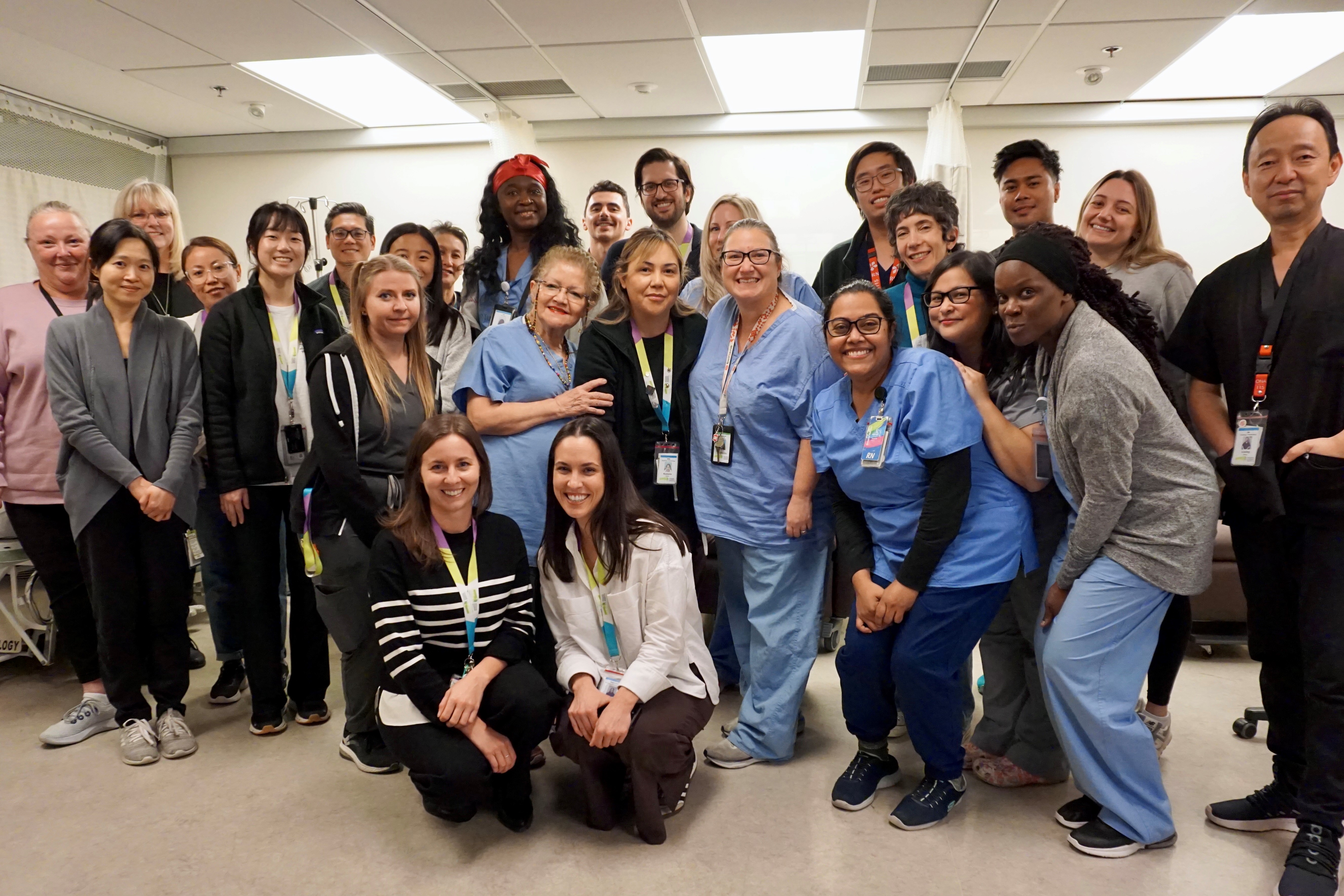
Recently, we had an opportunity to speak with the outstanding team at Michael Garron Hospital’s (MGH) Oncology & Hematology Clinic. What we heard from them, about their commitment and their determination to elevate patient safety each day, is something we knew we had to share with all of you.
Now, in the spirit of recognition and appreciation, we are proud to name MGH’s Oncology & Hematology Clinic an official HIROC Healthcare Change Maker! As you’ll learn in the story below, their dedication to highly reliable processes, willingness to adopt new practices, and culture of speaking up stands as an inspiring example for care teams everywhere.
Meanwhile, want to know what a Healthcare Change Maker is? Learn more.
Our hope is that their story sparks new ideas and inspires others across our healthcare system to take bold steps toward safer care.
Here’s what they had to say…
Why is celebrating patient safety important to the team at MGH / TEHN?
Our clinic's culture has a strong focus on high-reliability, systems design and patient safety. Over the past year, we have placed a special focus on patient safety and quality improvement. We have welcomed these changes with enthusiasm, engagement, and a genuine commitment to improve care for our patients and our team.
Here are some of the things we’ve accomplished:
- We have updated infusion practices to ensure the delivery of safe and effective treatment.
- We have implemented independent double checks to enhance safety.
- We have had two of our staff accepted into a Toronto Academic Health Sciences Network (TAHSN) Quality Improvement Fellowship, looking at improving care for oncology patients by:
- improving patient education and early recognition and intervention for toxicities/side-effects, and
- improving dietetic care for oncology patients.
- We have expanded our team to support the enhancement of safety and quality of care for patients on active treatment, including new clinical roles and a dedicated Nursing Education and Practice Lead.
- We have updated our team huddles with a structured approach and opportunities for staff to identify quality improvement and/or patient safety opportunities, and shout out colleagues for exemplifying excellent safety behaviours.
Has there been a safety success story over the past year that you can share?
One notable example of our safety culture is when our staff flagged an issue with some of the IV lines on the unit.
Our staff reported four events in which the lines were leaking and/or spilling. These incidents were flagged as 'good catch/near miss/no harm incident' which means they did not result in any injuries or consequences, but they were flagged as a concern given the potential for harm.
For example, our unit provides chemotherapy, which is cytotoxic and hazardous if exposure occurs. We did not want the issue with our impacted IVs to result in patient harm.
Because our staff were proactive in flagging these issues, we were able to implement mitigation strategies quickly, such as checking batch codes for the impacted lines, ensuring impacted lines weren’t being used in high-risk settings, and double-checking lines again before infusions. Our leaders were also responsive and appropriately supported escalation for a high-risk potential event.
Because of their combined and careful efforts, we have had zero incidents with harm to a patient!
What has made you so successful in sustaining a culture of safety?
We have supportive leadership who have had training and experience in developing high-reliability organizations and a culture of patient safety.
Staff are encouraged to speak up, new processes are co-designed with staff and patients, communication structures are in place to support daily rounding, huddles, and escalation of issues for timely resolution, and leaders listen and support safe practices.
Staff have also embraced a culture of learning and feel empowered to raise concerns.
A nurse once said that when she saw a practice she was unfamiliar with, she asked herself, “Is this just different or is it wrong?” This has become a mantra for our team – if there is a nagging question, just ask! That way, we can confirm if it’s just different. And if it’s wrong, we can fix it.
There is strong encouragement on our unit to ask questions, and staff are thanked for asking or clarifying something that may be incorrect or a patient safety issue.
Our staff are a tight-knit group and care deeply about their patients and one another. There are strong relationships between them all and a deep reciprocal relationship with our patients, who we see throughout the course of their medical oncological care. This has built a strong commitment to improving care where it matters.
Staff continue to be deeply compassionate and knowledgeable, and don’t shy away from asking hard questions, knowing that the result could make a difference for their patients. They celebrate each other’s successes, recognize and shout out safety behaviours on a regular basis, and are also comfortable giving us feedback along the way.
