Bluewater Health and the Quadruple-Aim
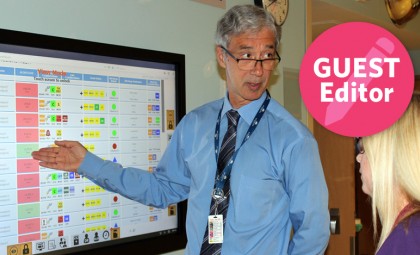
Mike Lapaine, President and CEO of Bluewater Health, on Building Strong, Respectful Relationships
March 7, 2019
As healthcare leaders, in the last decade we have become focused on monitoring outcomes, reducing risks, tracking data, and evidence-based decision making. This has value in moving us from narrow perceptions to facts, and in demonstrating our performance, identifying trends and evaluating new processes.
But to make the large changes we need at our hospitals and in the healthcare system, we have to engage in difficult conversations. We may also make assumptions about how to ‘fix’ issues in our hospitals, but if we don’t validate these assumptions with others, we can move forward in error. Finally, successful patient transitions require collaboration between different organizations in the healthcare system. All require strong, respectful relationships.
At Bluewater Health, a mid-sized community hospital located in Sarnia and Petrolia, we have built robust relationships with some early successes. We began with a focus on strengthening internal hospital relationships, between employees, physicians and leadership, and between different areas of the hospital. Many hospitals subscribe to the Triple-Aim: improve the health of the population, improve patient experience and reduce costs. We learned through our research the effect of employee engagement on all three goals, and a third-party employee survey conducted in 2016 revealed room for improvement in this area. The newer Quadruple-Aim focusses also on the provider or caregiver experience.
Our strategy was to create a culture of kindness with individuals and across teams, through an increased focus on employee well-being and acknowledging employees who make outstanding efforts. A commitment to maintaining training opportunities as an investment in people was folded into this cultural shift. A Culture of Kindness Employee Council was established that encouraged individuals and teams to recognize others, with many enthusiastic approaches: pharmacists offer ‘prescription refills’ on acts of kindness, the Dietary team has a Random Acts of Kindness Cart that brings treats to staff who do something kind.
Over two years, we have seen employee engagement improve significantly. Positive responses for the “hospital as a place to work” increased from 69.8 per cent to 76.3 per cent, and positive responses to “Can trust this organization” increased by 4.2 per cent.
Patient experience scores have been affected positively as well. They rose from 47 per cent to 55 per cent for Emergency Department patients, and from 66 per cent to 73 per cent for general hospital patients. These demonstrate significant improvement in areas that are often difficult to shift. The related rising patient experience scores have occurred during a time we have also been formalizing a relationship with some of our patients and family members: Patient Experience Partners (PEPs) are specially-trained volunteers who represent patients and families on committees throughout Bluewater Health, including Board committees and the Quality and Patient Experience Committee. PEPs also provide feedback on improvement initiatives and patient communications (e.g. scripts for Patient Discharge Follow Up phone calls). By integrating these patient and family representatives, we are able not only to listen, but to develop relationships and truly begin to see the hospital through the patient perspective, and co-develop solutions to provide better patient-centred care.
This is just one way that relationships have started to change our mindsets. Hospitals, like many other healthcare organizations, have many entrenched views, and a historical culture rooted in a hierarchical medical model. Now our healthcare system is in a period of disseminating power, and developing new models based on relationships between equals.
This has also been our experience as Bluewater Health entered into an Indigenous Partnership with Aamjiwnaang First Nation, Walpole Island First Nation, and Chippewas of Kettle and Stony Point First Nation, communities near Sarnia whose members are served by the hospital. The Partnership has helped us to understand ‘safety’ in a different way; we’ve been introduced to the concept of ‘cultural safety’ – an approach to creating an environment that is safe for Indigenous peoples, whereby they feel respected and receive quality healthcare that is nondiscriminatory. Together, we identified the value of establishing an Indigenous Patient Navigator position, and the role was filled in the spring of 2018.
Nowhere are relationships more important than in patient transitions, the Achilles heel of our system, where vulnerable patients may fall through the cracks, get sicker and return to the hospital. In an attempt to improve on this, some of the hard data used to evaluate hospitals includes re-admission rates. But this metric relies significantly on the work of external partners.
This is especially true in Mental Health and Addictions, an area that requires an integrated strategy between hospitals, primary care and community services. Relationships are vital to this integration, enhancing communication and establishing trust. At Bluewater Health, we developed a relationship with our local Canadian Mental Health Association Lambton Kent to the extent that we have entered into an exciting and unique partnership: we established the role of Integrated Vice-President, Mental Health and Addictions. This executive role is allowing us to integrate services and strengthen transitions. This has speeded up decision-making, and we have seen re-admissions to the Emergency Department (ED) reduced. Our psychiatrists are out supporting primary care practitioners in new ways so that they, too, can be better prepared to help those patients in need, and further diverting ED admissions for those best served in the community.
Bluewater Health is proud of what we’ve accomplished in innovating for improved patient outcomes, experience and safety and reduced readmission rates. We’ve accomplished this through kindness and relationships with varied partners in our area. I would even go so far as to suggest that hospitals in mid-size or smaller communities have an innovation edge in this area: relationships may already exist between individuals, and we may be better positioned and more nimble due to our size.
Mike Lapaine is the President and CEO of Bluewater Health in Sarnia and Petrolia, Ontario.
