Risk Watch (Feb '18)
Selected research, publications, and resources to promote evidence-informed risk management in Canadian healthcare organizations. Prepared by HIROC. Some titles are open access while others may require a subscription or library access; the librarian at your organization may be able to assist you. Please contact [email protected] for assistance if required.
Communication / Safety Huddles

Donnelly L, Basta K, Dykes A, et al. Jt Comm J Qual Patient Saf. 2018 (January);44(1):43-51.
Article describing the Daily Operational Brief (DOB), developed by a large pediatric hospital system in the US to quickly identify care delivery and safety issues. The DOB follows a standardized three-part process: meeting kickoff; review of quality and safety metrics, patient volume and staffing assessment, readiness assessment, problem-solving accountability system; debrief. Biweekly meetings attended by senior leaders are conducted for complex issues to chart progress made to date. In the first year of operation, 1,101 quick hits were identified [mean time to resolution 3.4 days; most common contributing factor was work environmental (64%)] along with 53 complex issues [mean time to resolution 95 days; most common contributing factor was task & technology (58%)]. The standardized readiness assessment prompts and a complex issue checklist and template are included..
Incident Reporting

Archer S, Hull L, Soukup T, et al. BMJ Open. 2017 (online, December):1-16.
Systematic review of 110 studies, including nearly 30,000 participants to identify factors contributing to patient safety incident reporting. In total, 748 barriers to incident reporting were identified compared to 372 facilitators. The top barriers were fear of adverse consequences (22%) and process and systems of reporting (15%), while the top facilitators were organisational factors (26%) and process and systems of reporting (20%). Authors noted that fear of adverse consequences and ineffective processes/systems of reporting should be high-priority areas that require consideration to improve engagement in incident reporting and ultimately learning from patient safety incidents.
Deteriorating Patient / Rapid Response Systems

Chua W, See M, Legio-Quigley H, et al. Int J Qual Health Care. 2017 (December);29(8):981-998.
Systematic review of 30 studies to describe the factors influencing activation of rapid response systems (RRS) by ward nurses and junior physicians. Using the Systems Engineering Initiative for Patient Safety model to understand the barriers and facilitators to activations of RRS, it was found factors influencing RRS activation were spread across four components: persons, tools and technologies, tasks, and organization. This included frontline clinicians’ perception of RRS and their clinical judgment, support from colleagues and hospital leaders, adequacy of activation criteria, attitudes and responses of rapid response team members, adherence to traditional models of escalation of care, and staff training and education. Authors noted organizations considering adopting or improving RRS should consider the complex interactions between people and technologies, tasks and organization. Tables explaining the factors identified are provided.
Information Gaps / Test Results
Patient perceptions of receiving test results via online portals: a mixedmethods study

Giardina T, Baldwin J, Nystrom D, et al. J Am Med Inform Assoc. 2017 (online, December):1-7.
Study to explore patients’ experiences and preferences when accessing their test results in patient portals. Interviews were conducted with 95 patients who viewed a test result over a 17 month period at four large outpatient clinics in the US. Results identified 63% did not receive any explanatory information or test result interpretation at the time they received the result and 46% conducted online searches for further information. Patients who received an abnormal result were more likely to experience negative emotions and to call their physician (44%) than those who received a normal result (15%). Overall, a quarter of participants sent a secure message to their doctor regarding the test result. Authors noted online portals are not currently designed to present test results to patients in a meaningful way and patients experience negative emotions often with abnormal results and sometimes with normal results. Key recommendations are provided for improving the design and use of patient portals.
Medication / Opiods
Persistent opioid use among pediatric patients after surgery

Harbaugh C, Lee J, Hu H, et al. Pediatrics. 2017 (online ahead of print, December):1-8.
Retrospective cohort study to examine if increased incidence of prolonged opioid prescription refills occur among adolescents and young adults who received opioids after surgery in the US. Data from a four year period of opioid-naive patients ages 13 to 21 who underwent one of thirteen operations was reviewed. The surgical group was compared to a random sample nonsurgical patient control group who were opioid-naive. Results identified in the surgical group that 60.5% of patients (88,637) filled a postoperative opioid prescription. Persistent opioid use was found in 4.8% (4,267 patients) of the patient surgical group filling prescriptions between 90 days and 180 days after surgery compared with 0.1% of the non-surgical group. Patients with persistent opioid prescriptions filled a substantial quantity. Cholecystectomy and colectomy were associated with the highest risks of persistent opioid use. Independent risk factors included older age, female sex, previous substance use disorder, chronic pain, and preoperative opioid fill.
Communication / Neonatal

Sundgren N, Kelly F, Weber E, et al. BMJ Open Qual. 2017 (online, December):1-6.
Quality improvement project in a US hospital with the aim to increase the frequency that summoning pages to the neonatal resuscitation team (NRT) contained specific information of the gestational age and reason for the attendance to be included greater than 90% of the time. Authors identified timeliness and information contained in the page help the NRT to optimally prepare for post-delivery infant care. At baseline, based on 229 pages, 8% of pages contained gestational age and 33% of pages contained a reason for NRT attendance. Following plan-do-study-act cycles over an eight month improvement period, results showed percentages increased to 97% for gestational age and for the reason for NRT attendance. Balancing measures were chosen to ensure the use of the paging tool did not increase the time it took to communicate the information and subsequently, the timely arrival of the NRT to deliveries. Measures of page timeliness did not change. Authors concluded paging communication between obstetric and the NRT is crucial for optimal perinatal outcomes.
Risk Management / Controls
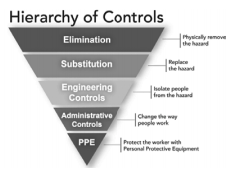
Liberati E, Peerally M, Dixon-Woods M. Int J Qual Health Care. 2017 (online ahead of print, December):1-5.
Study to examine the hierarchies of risk controls approach (five tiers), familiar to high-risk industries, for its appropriateness for healthcare across four UK hospitals. The least effective intervention is ‘personal protective equipment’ with the most effective intervention being ‘elimination’. Results showed a total of 42 risk controls aimed at addressing safety hazards; most (35) of these were classified as ‘administrative’ controls, which are considered weak interventions. The remaining controls were classified as ‘engineering’ (6) or ‘substitution’ controls (1), with ‘substitution’ being the strongest type of intervention. Authors noted three issues related to use of the hierarchy: categorization of interventions based on superficial and visible characteristics; failure to take into account the fit between the identified hazards and the planned interventions; and poor relation to the social and organizational factors that contribute to safety interventions.
Leadership / Culture
Promising practices for improving hospital patient safety culture

Campione J, Famolaro T. Jt Comm J Qual Patient Saf. 2018 (January);44(1):23-32.
Study to understand promising best practices to improve patient safety culture across acute care hospitals in the US, as identified by the Agency for Healthcare Research and Quality Surveys on Patient Safety Culture Hospital Survey database. Results showed a 1.7 percentage point increase in the mean change in the all-composite percent positive culture score of 536 hospitals. The six top-improving hospitals had an average increase of 8.6 percentage points in their culture score. The six top-improving hospitals shared three common practices: goal setting and strong action planning for quality improvement; implementation of well-known patient safety initiatives and programs (e.g. Patient Safety Leadership Walkabouts); and rigorous survey administration methods. Other best practices included: leadership support and hospital focus on organizational culture; quality improvement; importance of assessing patient safety culture; consistent patient safety manager over time; importance of middle management in patient safety culture improvement; and ease, promotion and root cause analysis feedback related to event reporting.
Mortality / Patient safety

Bai A, Srivastava S, Tomlinson G, et al. BMJ Qual Saf. 2018 (January);27(1):11-20.
Study to compare in-hospital mortality of general internal medicine (GIM) patients bedspaced to off-service wards with GIM inpatients admitted to assigned GIM wards at a Canadian tertiary care hospital. Of 3,243 patients, results showed 35% of GIM admissions were bedspaced to off-service wards with the remaining 65% admitted to assigned GIM wards. Five percent of patients died in hospital including 88 bedspaced patients and 88 assigned to GIM wards. Bedspaced patients had significantly greater in-hospital mortality than assigned GIM ward patients, which decreased per day in hospital. Authors noted the importance of managing patient flow and bed mapping so that patients get to the appropriately assigned ward.
Other Resources of Interest
Closing the loop: a guide to safer ambulatory referrals in the EHR era (December 2017). Institute for Healthcare Improvement/National Patient Safety Foundation (US) guide to optimize the reliability of referrals.
Dying in the hospital with advanced dementia (December 2017). Agency for Healthcare Research and Quality (US) web M&M case about a patient with dementia whose goals for end of life care were not met.
Four risks healthcare executives should monitor in 2018 (December 2017). Managed Healthcare Executive (US) article; top risks are the opioid crisis, missed and/or delayed infection diagnoses, violence and long-time staff.
How boards can reduce corporate misbehavior (December 2017). Harvard Business Review (US) article outlining a tenstep program to help boards reduce the risks of illegal behavior, reinforce ethical conduct, and enhance reputation.
Miscommunication in the OR leads to anticoagulation mishap (December 2017). Agency for Healthcare Research and Quality (US) web M&M case on a communication error due to an omitted step of the surgical safety checklist.
Rabble-rousing surgical staff wear their names on their caps to stop mix-ups and improve patient safety (December 2017). Sydney Morning Herald (AUS) article including pictures of surgical cap naming to improve safety.
Revised never events policy and framework (January 2018). NHS Improvement (UK) revised policy and framework; includes 16 events related to surgery, medication, mental health, general categories.
Stop the world, I want to improve: governing for quality improvement when there’s no ‘off switch’ (December 2017). The Health Foundation (UK) blog article on how boards govern for quality improvement.
Surgical fires: nightmarish “never events” persist (January 2018). Canadian Medical Association Journal news article outlining review of 54 cases of perioperative burns by the Canadian Medical Protective Association.
Toolkit to promote safe surgery (December 2017). Agency for Healthcare Research and Quality (US) resource for perioperative and surgical units to prevent surgical site infections.
Top 10 legal risks for business in 2018 (January 2018). Borden Ladner Gervais LLP (CDN) report of top risks; risks include cybersecurity, privacy and data protection; market implications of legalizing cannabis; and class actions.